Navigating AI in Healthcare
We take pride in helping people from all walks of life understand the impact and potential benefits of AI in Healthcare and to help end the stigma!
How we deal with the rise of AI
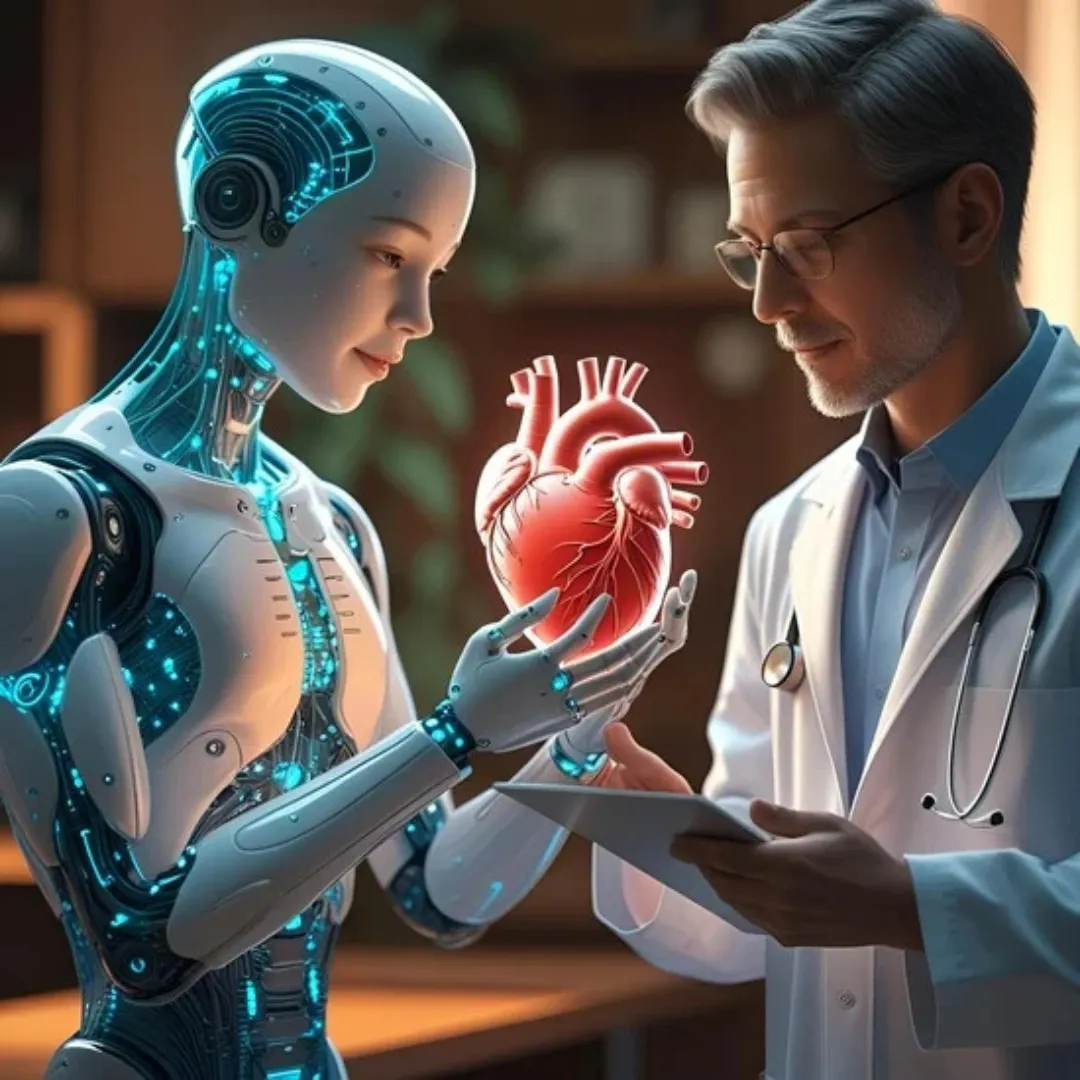
Harnessing the Rise of AI to Serve You Better
Our clients are our top priority. We are in constant communication with the providers we serve and are committed to advancing the immediate needs and wants of our clients. Our team works around the clock to provide the necessary services and support that each client needs from us and thanks to AI its easier than ever!
Who is Dr. Joe?
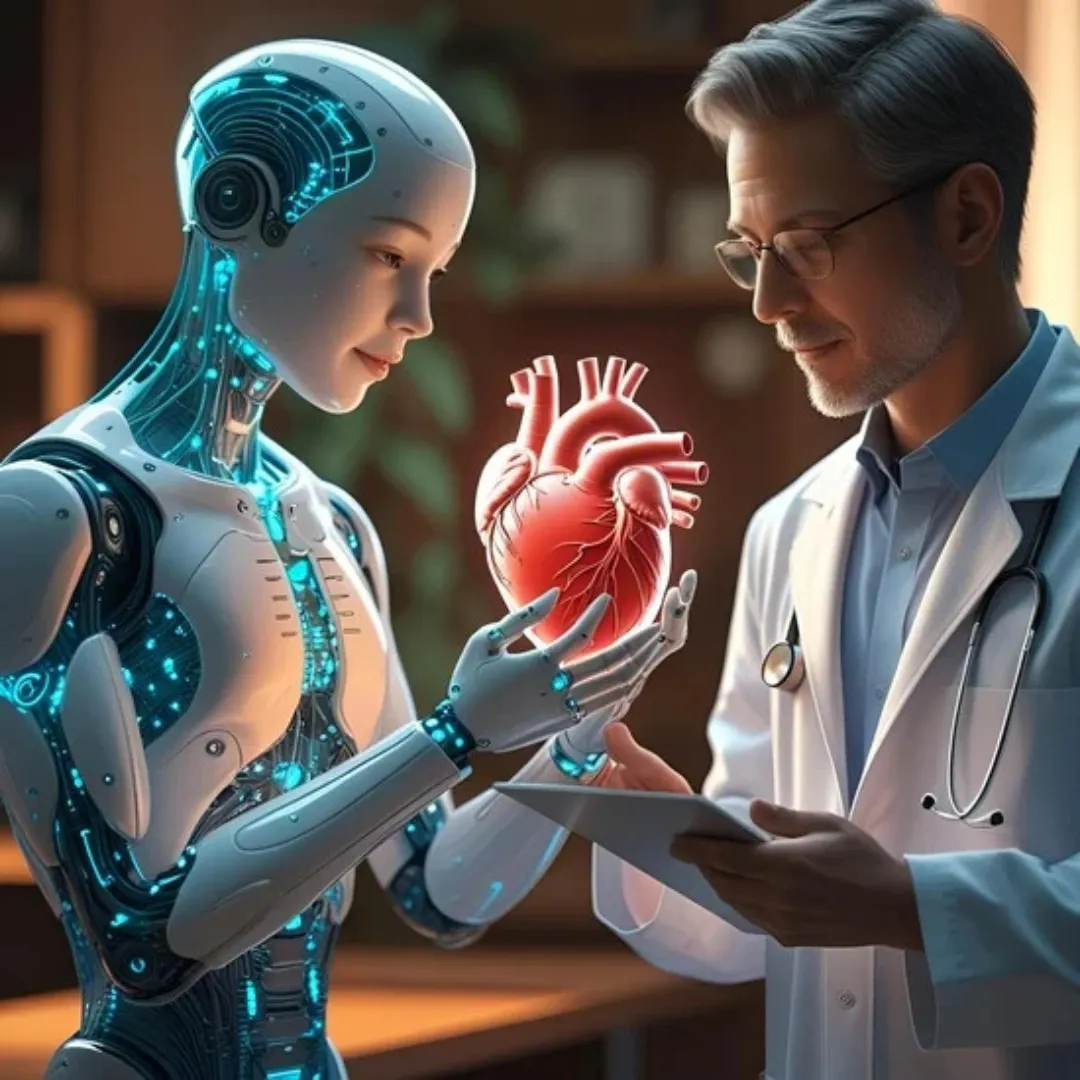
Dr. Joe 2.0: Where Healing Meets Intelligence
Dr. Joseph Rosado is a pioneering physician at the intersection of integrative medicine and artificial intelligence. With decades of experience in functional and regenerative health. He’s now leading a new movement: smarter, tech-enabled healing.
Through education, innovation, and clinical insight, Dr. Joe helps practitioners and patients embrace the future of medicine with clarity, efficiency, and care.

Our Services

Let’s demystify artificial intelligence and turn it into a powerful ally in your clinic or coaching practice. From automated charting to brand-building—I'll guide you step-by-step.

Private Practice Automation
GPT Tool Training
Brand Strategy & Tech Integration
Aging Gracefully with AI
About Dr. Joe
I’m Dr. Joe Rosado, a physician, educator, and innovator fusing functional medicine with artificial intelligence. I help health professionals harness cutting-edge tools to elevate care, reduce burnout, and future-proof their practice.
Physician. Visionary. AI Advocate for Healers.
Author. Speaker. Mentor.
When I’m not working towards my next adventure, I enjoy playing golfing, doing martial arts, being a foodie, spending time with my twin daughters and grandchildren, and like to enjoy a good cigar on occasion.

Frequently asked
questions
Who is your service for?
We serve private practices, clinics, health coaches, and integrative medicine practitioners who want to use AI tools more effectively—for charting, client communications, branding, workflow, etc.
Is patient data safe when using AI tools?
Yes. We prioritize privacy and security. We follow best practices for handling sensitive health information, complying with laws/regulations, using secure systems, and ensuring data is only used with consent.
Do you provide training/support for using AI tools?
Yes. We offer hands-on training (for you or your team) on selecting, using, integrating, and maintaining AI tools, with ongoing support so you’re not left alone after setup.
How long before I see results in my practice?
It depends on your starting point (current workflow, tech readiness, team). But many clients report noticeable improvements in efficiency, time savings, and reduced admin burden within a few weeks to a few months.
What is the cost of working with Dr. Joe 2.0’s services?
Costs vary depending on the service, size of your practice, and the scope of work. We offer different packages and custom plans. Contact us for a quote tailored to your needs.
How do I get started?
Just reach out! We’ll set up a consultation to understand your goals, offer recommendations, map out a plan, and then help with implementation, training, and ongoing improvement.
Contact us via support if you have any more questions.
Innovation
Fresh, creative solutions.
Integrity
Honesty and transparency.
Excellence
Top-notch services.
