When Your Mind Feels Foggy—It Might Be Depression

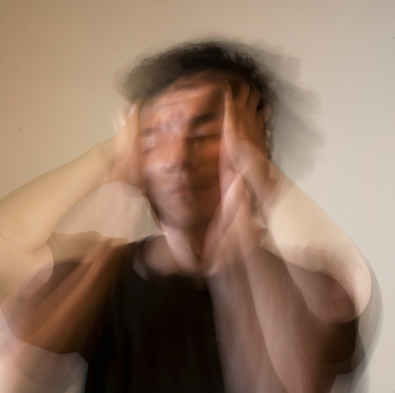
Forgetting appointments, losing your train of thought, struggling to recall simple words—these cognitive hiccups are more than just frustrating. For many people living with depression, memory loss isn’t just an inconvenience—it’s part of the condition.
Depression doesn’t only affect mood. It changes how your brain processes, stores, and retrieves information. And while this symptom is often overlooked, it can have a serious impact on daily functioning, work, relationships, and self-confidence.
How Depression Affects the Brain

Depression is more than just feeling sad. It causes real changes in the brain’s structure, chemistry, and function—especially in areas responsible for memory and attention. These include:
- Hippocampus: Critical for memory formation; often smaller in those with chronic depression.
- Prefrontal Cortex: Manages attention, decision-making, and working memory.
- Amygdala: Involved in emotion processing and emotional memory—often overactive in depression.
Chronic stress and inflammation—both linked to depression—can also disrupt neuroplasticity, the brain’s ability to form and maintain connections.
Types of Memory Affected by Depression

Depression doesn’t cause the same type of memory loss as conditions like Alzheimer’s—but the effects are very real. Common complaints include:
Trouble holding information in your mind short-term—like remembering why you walked into a room or losing track of a conversation.
Difficulty recalling recent events or conversations, leading to repeated questions or forgotten tasks.
Struggling to find the right word, recall names, or follow detailed instructions.
Memory issues are often worsened by lack of focus. Depression makes it hard to concentrate, which means your brain never fully records information to begin with.
Why It Feels So Frustrating

These cognitive symptoms can feel deeply unsettling—especially if you’re typically organized, articulate, or high-functioning. Many people with depression fear they’re “losing their mind” or developing dementia, when in fact:
- The brain is exhausted from emotional overload
- Stress hormones are impairing recall and focus
- Sleep disturbances (common in depression) are reducing memory consolidation
It’s not that you’re careless or failing. Your brain is overwhelmed—and doing its best to keep up.
Can Depression-Related Memory Loss Improve?
When depression is treated effectively, memory and concentration often return to normal—or improve significantly. But this requires addressing both the mood disorder and the cognitive symptoms together.
Therapy, medication, and lifestyle changes like better sleep, nutrition, and movement can all support cognitive recovery. In some cases, targeted cognitive training or neuroplasticity-based therapies may also help rebuild mental sharpness. The key is to treat the root cause—not just the brain fog. With the right support, clarity and confidence can return.
Ways to Support Cognitive Function While Managing Depression
Therapy, antidepressants, ketamine therapy, or other physician-recommended treatments can help restore neurotransmitter balance and improve cognitive function over time.
Brain games, reading, puzzles, and journaling can stimulate memory and sharpen focus—even during periods of low mood.
Depression often disrupts sleep—and poor sleep severely impacts memory. Regular bedtimes, reduced screen time, and a calming routine can help.
Exercise boosts blood flow to the brain, enhances memory, and improves mood. Even light movement like walking or stretching can be beneficial.
When your brain is tired, external supports help. Try:
- Setting calendar alerts
- Keeping task lists
- Using sticky notes or phone reminders
Low levels of B12, omega-3s, and vitamin D can impact brain health. A professional can help assess whether supplements or dietary changes are needed.
When to Seek Help

If memory issues are interfering with your ability to function, connect with others, or feel confident in daily tasks, it’s time to seek professional support—especially if they come alongside feelings of hopelessness, fatigue, or emotional detachment. These aren’t just “bad days” or signs of getting older; they may be symptoms of depression affecting how your brain operates.
You don’t have to wait for things to get worse. The sooner you address these changes, the better your chances of reversing them. With timely, compassionate care, recovery is possible—and so is feeling mentally sharp, emotionally balanced, and fully yourself again.
Frequently Asked Questions (FAQs)
Depression typically affects short-term and working memory, not long-term memory. With proper treatment, memory often improves.
Yes. Anxiety and depression can both impair focus, which in turn affects memory recall.
A mental health provider can assess whether your memory issues are depression-related or suggest further evaluation if needed.
For many, yes. By improving mood, antidepressants can also improve concentration and memory. But some people may experience mild cognitive side effects—discuss any concerns with your doctor.
Brain fog is a general sense of confusion or mental fatigue. Memory loss refers to specific lapses in recall. Both are common in depression.
Indirectly, yes. Therapy reduces emotional stress, improves coping skills, and helps address the root of cognitive symptoms.
Absolutely. Sleep is essential for memory consolidation. Depression-related insomnia or hypersomnia can impair recall and mental clarity.
Yes. Struggling with memory can lead to frustration, shame, and fear—often reinforcing depressive symptoms. Addressing both is key to recovery.
A psychiatrist or mental health-informed primary care doctor is a good place to start. They can rule out other causes and begin treatment for depression.
Final Thoughts: Your Brain Isn’t Broken—It’s Asking for Help

Memory lapses, mental fog, and lack of focus aren’t signs of failure—they’re signals that your brain is under pressure and needs support. These experiences are common in depression and deserve to be acknowledged, not minimized.
With compassionate care and the right treatment, cognitive clarity can return. Emotional weight can ease. And each small step forward can help restore not just your memory, but your overall sense of well-being.