Understanding the Difference: Two Faces of Depression

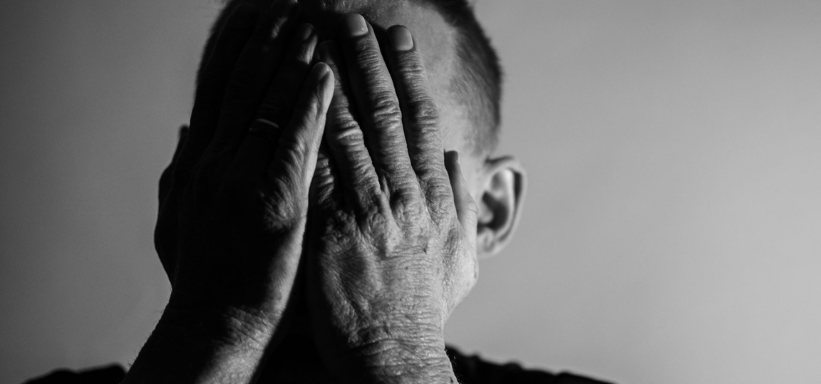
Depression doesn’t always look or feel the same. Major Depressive Disorder (MDD) often appears suddenly, with intense symptoms that disrupt daily life. In contrast, dysthymia—also known as Persistent Depressive Disorder—develops gradually and lingers in the background, creating a long-term sense of emotional dullness or fatigue.
Recognizing which type you’re experiencing can make a meaningful difference in how you approach treatment, manage symptoms, and support your mental well-being over time.
What Is Dysthymia (Persistent Depressive Disorder)?

Dysthymia is a long-lasting, chronic form of depression. It often feels like a low-grade emotional fog that never quite lifts.
Symptoms of Dysthymia Include:
- Feeling low or “flat” most of the time
- Difficulty experiencing joy, even during happy events
- Low self-esteem or chronic self-criticism
- Ongoing fatigue and low energy
- Sleep and appetite changes
- Difficulty concentrating or making decisions
To be diagnosed, symptoms must persist for at least two years in adults (or one year in adolescents).
What Is Major Depressive Disorder (MDD)?

Major depression involves more severe symptoms that may occur in episodes lasting weeks or months. These episodes interfere significantly with daily functioning.
Symptoms of MDD Include:
- Intense sadness, hopelessness, or emotional numbness
- Loss of interest in nearly all activities
- Thoughts of worthlessness, guilt, or suicide
- Changes in appetite or weight
- Insomnia or excessive sleeping
- Restlessness or slowed physical movement
- Difficulty focusing or making decisions
Major Depressive Disorder (MDD) may arise abruptly, sometimes following a significant life event—but it can also develop gradually, without any obvious cause.
Key Differences Between Dysthymia and Major Depression
Feature | Dysthymia (PDD) | Major Depressive Disorder (MDD) |
Duration | At least 2 years | At least 2 weeks |
Intensity | Low to moderate but chronic | Moderate to severe and episodic |
Symptom Pattern | Persistent, ongoing mood disturbance | Periodic episodes with potential remission |
Energy Level | Mild fatigue | Significant fatigue or restlessness |
Impact on Daily Life | Subtle but long-term impairment | Noticeable, immediate disruption |
Why Diagnosis Matters
Dysthymia is often misdiagnosed or ignored because people normalize feeling “off” for long periods. On the other hand, MDD may be overlooked if someone isn’t in acute crisis but is still struggling internally.
Without the right diagnosis:
- People with dysthymia may never seek treatment, thinking this is “just how life feels”
- People with MDD may go untreated during crucial moments of risk
Accurate diagnosis leads to better outcomes, faster relief, and more sustainable care.
Treatment Options for Both Conditions
For Dysthymia:
- Cognitive Behavioral Therapy (CBT)
- Lifestyle changes (movement, sleep, nutrition)
- SSRIs or other antidepressants (long-term use may be needed)
- Mindfulness or Acceptance & Commitment Therapy
For Major Depression:
- Antidepressant medication (SSRIs, SNRIs, etc.)
- Structured psychotherapy (CBT, psychodynamic therapy, EMDR)
- Advanced interventions for treatment-resistant depression (e.g., ketamine therapy)
- Support groups or intensive outpatient programs
When You Might Be Dealing with Both


Some individuals experience double depression—a chronic baseline of dysthymia that periodically deepens into major depressive episodes. This layering can make symptoms feel especially heavy and prolonged. It also complicates treatment if not accurately identified. That’s why it’s so important to track emotional patterns over time and seek a professional evaluation. Understanding whether you’re dealing with one condition or both helps guide more effective, comprehensive care—and brings you closer to relief that lasts.
Frequently Asked Questions (FAQs)
Yes. It’s common for someone with dysthymia to experience a major depressive episode on top of their chronic low mood.
Not exactly. While the symptoms are often less intense, the chronic nature of dysthymia can be just as debilitating in the long run.
If you’ve felt emotionally “off” or persistently low for more than two years without full remission, it may be dysthymia.
Yes. Antidepressants can be effective for both, though medication alone is often more effective when combined with therapy.
The core techniques may overlap, but dysthymia often requires a longer-term approach that focuses on emotional resilience and identity repair.
High-functioning depression is real. Share what you feel internally, not just what others see on the outside.
Yes—though they’re not cures, regular movement, quality sleep, and social connection can boost treatment outcomes.
Both dysthymia and MDD can worsen over time, potentially leading to increased risk of suicidal thoughts, health issues, and loss of functioning.
Yes. With proper care, many people recover fully and regain a sense of emotional balance and well-being.
Final Thoughts: Every Form of Depression Deserves Attention

Whether you’re facing a steady, low-grade heaviness or the intense weight of a depressive episode, both experiences deserve clinical attention and compassionate care. Depression shows up differently for everyone—but in all its forms, it’s real, valid, and treatable.
Identifying what you’re experiencing is a powerful first move. With expert support and evidence-based care, you can start to feel grounded, capable, and connected again. You don’t have to manage this on your own.