Imagine waking up each morning, feeling a sharp ache in your knee or a dull stiffness in your shoulder. Over time, the pain makes it harder to walk, climb stairs, or even enjoy simple activities like gardening or playing with your kids. If this sounds familiar, you’re not alone.
Joint pain affects millions of people worldwide, making everyday movements uncomfortable or even unbearable. Whether caused by aging, arthritis, sports injuries, or repetitive strain, joint pain can limit mobility and significantly impact quality of life.
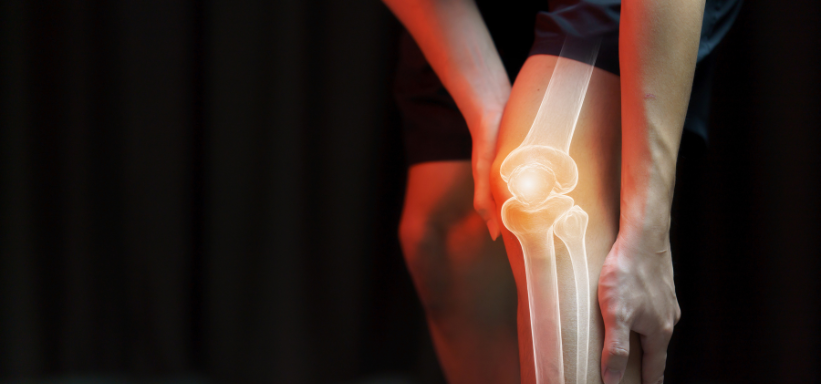
What Causes Joint Pain?
Joint pain isn’t always the result of a single injury—it can develop over time due to:
- Osteoarthritis: Wear and tear on the joints, leading to cartilage breakdown.
- Rheumatoid Arthritis: An autoimmune condition that causes inflammation and joint damage.
- Tendon or Ligament Injuries: Strains, sprains, or tears that make movement painful.
- Post-Surgical Recovery: Some individuals experience lingering pain after surgery.
Many treatments aim to manage pain, but some only provide temporary relief. This is where Platelet-Rich Plasma (PRP) Therapy is changing the landscape of joint pain management.
Wouldn’t it be great if there were a way to tap into your body’s natural healing ability? That’s exactly what PRP therapy does. Let’s explore how it works and why it’s gaining popularity among those seeking lasting pain relief.
How PRP Works for Joint Pain
- Blood is drawn from your arm, similar to a routine blood test.
- The blood is placed in a centrifuge, which spins at high speeds to separate and concentrate the platelets.
- The platelet-rich solution is injected directly into the painful joint.
- Growth factors begin the healing process, reducing inflammation and promoting tissue regeneration over time.
Unlike traditional treatments that mask pain, PRP therapy addresses the root cause by enhancing the body’s natural repair mechanisms. But what makes it stand out compared to other treatment options?
Benefits of PRP Therapy for Joint Pain
Many people wonder, “Is PRP just another trend, or does it truly work?” While research is still ongoing, multiple studies and patient experiences suggest that PRP therapy offers several key benefits:
1. Pain Relief and Inflammation Reduction
2. Improved Joint Function and Mobility
3. Natural Healing and Regeneration
4. Minimally Invasive with Little Downtime


The PRP Treatment Process: What to Expect
If you’re considering PRP therapy, knowing what to expect can help ease any concerns. The procedure is relatively simple and completed in under an hour. Here’s a step-by-step breakdown:
Step 1: Blood Collection
A small amount of blood is drawn from your arm—similar to a routine lab test. This is the first step in preparing the platelet-rich solution for your treatment.
Step 2: Platelet Separation
The blood is placed in a centrifuge, a machine that spins rapidly to separate platelets from other blood components. The resulting concentrated PRP solution is what makes this therapy effective.
Step 3: PRP Injection into the Joint
Once prepared, the PRP is carefully injected into the affected joint using ultrasound guidance for accuracy. This ensures the platelets reach the precise area where healing is needed.
Step 4: Recovery and Aftercare
- Mild soreness at the injection site is common but typically fades within a few days.
- Light movement is encouraged, but strenuous activities should be avoided for the first week.
- Healing occurs gradually, with improvements noticeable within a few weeks to months.
Most patients require one to three sessions depending on the severity of their joint pain. Unlike medications that provide only short-term relief, PRP promotes lasting healing by addressing the root cause of the pain.
Who Can Benefit from PRP Therapy?
PRP therapy isn’t just for elite athletes or those recovering from surgery—it’s becoming a go-to solution for anyone struggling with persistent joint pain. But is it right for you?
Ideal Candidates for PRP Therapy
PRP may be a good option if you:
✔ Experience chronic joint pain due to arthritis or wear and tear
✔ Have suffered sports injuries or repetitive stress damage
✔ Want to avoid surgery and explore non-invasive treatments
✔ Have tried other treatments (like cortisone injections) with little success
✔ Are looking for a natural approach that harnesses the body’s healing ability
Conditions That PRP Can Help Treat
PRP is commonly used for:
- Osteoarthritis (Knee, Shoulder, Hip, and Ankle) – PRP helps slow cartilage breakdown and reduces inflammation.
- Tendonitis & Ligament Injuries – A great option for tennis elbow, rotator cuff injuries, and Achilles tendonitis.
- Meniscus Tears & Cartilage Damage – Supports healing in small tears and slows the progression of joint degeneration.
- Post-Surgical Recovery – PRP is often used after orthopedic surgeries to enhance healing.
While PRP is highly effective for many, it’s not for everyone. Individuals with severe joint damage or advanced arthritis may need more intensive treatments like stem cell therapy or surgery. Consulting a PRP specialist can help determine the best course of action.
Now, how does PRP compare to other common treatments?
Comparing PRP to Other Joint Pain Treatments
If you’ve been managing joint pain for a while, you’ve likely come across cortisone injections, physical therapy, and even surgical options. So how does PRP measure up?
PRP vs. Cortisone Injections
- Cortisone: Provides short-term pain relief by reducing inflammation but doesn’t repair damaged tissue. Frequent injections may even weaken cartilage over time.
- PRP: Stimulates natural healing while reducing inflammation, providing longer-lasting relief without the risk of cartilage breakdown.
PRP vs. Surgery
- Surgery: Often recommended for severe cases but requires long recovery times and potential risks.
- PRP: A non-surgical option that can help delay or even prevent the need for surgery in many cases.
PRP vs. Physical Therapy
- Physical therapy: Helps improve strength and mobility but doesn’t always address underlying damage.
- PRP: Complements physical therapy by enhancing healing at a cellular level, making rehab more effective.
Which Treatment Is Right for You?
Choosing the right approach depends on your condition, lifestyle, and long-term goals. PRP is a great middle ground—less invasive than surgery but more regenerative than temporary pain relief treatments.
Still, PRP isn’t without controversy. Let’s address some of the common myths surrounding this treatment.
Common Myths and Misconceptions About PRP
Despite its growing popularity, PRP therapy is often misunderstood. Let’s clear up some of the most common myths.
1. “PRP is just a placebo—it doesn’t really work.”
Not true. Numerous studies have shown PRP to be effective in reducing pain and improving function. While results vary, many patients experience lasting relief when PRP is used appropriately.
2. “PRP works immediately.”
Unlike cortisone injections that offer instant relief, PRP takes time to work. Most patients see gradual improvement over several weeks to months as the body repairs itself.
3. “PRP is only for athletes.”
While PRP gained popularity in the sports world, it’s for anyone dealing with joint pain—from weekend warriors to seniors with arthritis.
4. “One PRP injection is all you need.”
Some people see significant improvement after a single treatment, but others may need multiple sessions depending on their condition and overall health.
5. “PRP is painful and has major side effects.”
PRP injections cause mild discomfort, similar to a flu shot, but most people tolerate it well. Since PRP is derived from your own blood, the risk of complications is extremely low.
Understanding the facts helps patients make informed decisions about their health. But what do real patients say about PRP? Let’s take a look.
PRP therapy has promising results, but it’s not for everyone. Understanding whether you’re a good candidate can help you set the right expectations.
You May Benefit from PRP If:
✔ You have mild to moderate joint pain that affects your daily life.
✔ You want a natural, regenerative approach instead of relying on painkillers.
✔ You have tried other treatments (physical therapy, cortisone shots) with little success.
✔ You are not ready for surgery and want to explore other options first.
✔ You lead an active lifestyle and need to maintain joint function.
PRP May Not Be Suitable If:
✘ Your joint damage is too advanced, such as severe osteoarthritis with complete cartilage loss.
✘ You have blood disorders or clotting conditions that prevent proper platelet extraction.
✘ You are on certain medications, like blood thinners, that interfere with PRP’s effectiveness.
✘ You expect instant relief—PRP takes time to show results.
If you’re unsure, the best approach is to consult a specialist who can assess your condition and recommend whether PRP is a viable option for you.